Skeletal muscle injury caused by any
mechanism (direct, genetic, biochemical) is termed as rhabdomyolysis. Injured muscle fibers release cellular contents into the circulation leading to myoglobinuria. Besides myoglobin, cellular contents also include enzymes suck as creatine kinase (CK), aldolase, LDH, AST, and potassium. Eventually, the Na+K+ATPase pump and Ca transport takes the hit resulting in increased intracellular calcium and muscle injury. Calcium also activates intracellular enzymes including proteases inducing production of free oxygen radicals.
Potential causes of rhabdomyolysis include:
 |
| Pathophysiology of Rhabdomyolysis |
Potential causes of rhabdomyolysis include:
- Alcohol (Prolonged immobilisation and direct alcohol related toxicity, Low K/Mg/PO4 also predispose)
- Recreational Drug use (Cocaine, Amphetamines, Opoids)
- Medications (Statins, TCAs, SSRIs, Lithium, Steroids, MAOi )
- Myopathies(Dermatomyositis, Polymyositis)
- Trauma (Electricity, Crush Injury)
- Seizures
- Prolonged Immobility (Post Falls in Elderly)
- Infection (Bacterial and Viral)
- Strenuous physical activity
- Heat-related illness.
Inherited metabolic
disorders should be suspected with recurrent episodes of rhabdomyolysis
Clinical Presentation
- Acute onset muscle aches
- Muscle stiffness and weakness
- Fever
- Dark coloured urine.
- Nausea, vomiting and tachycardia
- Tenderness Muscles
Examination may be completely normal. Therefore, look for cues in the history and work up based on that.
Diagnosis
Diagnosis
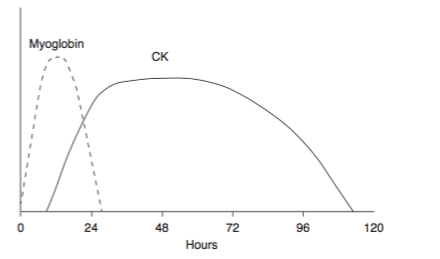
Raised CK is a marker of muscle injury. The degree of elevation correlates with the
amount of damage but it is unrelated with the morbidity. A rise in CK >5 times than normal is considered as significant. CK levels begin to rise 2 to 12 hours after the onset of injury, and peak within 24 to 72 hours.
 |
| Pattern of Myoglobin and CK rise during Rhabdomyolysis |
Myoglobin elevation actually occurs before CK elevation but it rapidly cleared from
the plasma. It enters urine only when the plasma concentration is significantly elevated. Because myoglobin
contains heme, dipstick tests may turn positive as then test cannot differentiate among hemoglobin,
myoglobin, and red blood cells. Therefore, suspect myoglobinuria
when the urine dipstick test is positive for blood but no red blood cells
are present on microscopic examination.
Myoglobin levels may return to
normal within 1 to 6 hours after the onset of muscle necrosis, therefore absence of an elevated serum myoglobin level or of myoglobinuria does
not exclude the diagnosis.
Due to cellular injury, serum electrolyte disturbances are seen commonly (Low Ca, High K/Uric Acid/Phosphorus). Renal Function tests reflect the extent of kidney injury.
Management
Management
- Treat the underlying cause
- Aggressive Fluid Resuscitation (Normal Saline)
- Target Urine Output is 200-300ml/hr (catheterise to check output in critically ill)
- Treat Hyperkalemia with usual measures
- Avoid Nephrotoxic Medications
- Renal Replacement therapy
- Consider mannitol, especially if compartment syndrome - Low grade evidence
As usual - Bicarbonate is recommended by some but without any definite evidence base.
The idea of urine arlkalinization stems from the fact that myoglobin precipitation is increased in acidic urine. However, in clinical studies - urine alkalinization
has not been shown to impact outcomes.
Compartment syndrome and peripheral nerve injury are potential mechanical complications of Rhabdomyolysis. Rarely, thromboplastin release from damaged
muscle leads to consumptive coagulopathy and DIC.
Take Home
References:
- Early recognition and prompt initiation of treatment is the key
- Pick cues from the history as examinations findings can be subtle or absent
- Watch for the complications (DIC, Compartment Syndrome)
References:
- Parekh R, Care DA, Tainter CR. Rhabdomyolysis: advances in diagnosis and treatment. Emergency medicine practice. 2012 Mar;14(3):1-5.
- Malinoski DJ, Slater MS, Mullins RJ. Crush injury and rhabdomyolysis. Critical care clinics. 2004 Jan 1;20(1):171-92.
- Giannoglou GD, Chatzizisis YS, Misirli G. The syndrome of rhabdomyolysis: pathophysiology and diagnosis. European journal of internal medicine. 2007 Mar 31;18(2):90-100.
- ThomasR:Towardsevidence-basedemergencymedicine: bestBETS from the Manchester Royal Infirmary. Emerg Med J 27: 305, 2010.
- Dalakas MC: Toxic and drug-induced myopathies. J Neurol Neurosurg Psychiatry 80: 832, 2009.
- Clarkson PM, Eichner ER: Exertional rhabdomyolysis: does elevated blood creatine kinase foretell renal failure? Curr Sports Med Rep 5: 57, 2006. [PMID: 16529674]
- Vanholder R, Sever MS, Ekrem E, et al: Rhabdomyolysis. J Am Soc Nephrol 11: 1553, 2000.
Posted by:
Lakshay Chanana
Speciality Doctor
Northwick Park Hospital
Department of Emergency Medicine
England

No comments:
Post a Comment