Management of accidental hypothermia has seen a revolution with the use of ECLS. ECLS has substantially improved survival and is the treatment of choice in the patient with unstable circulation or CA.The crucial factor in all hypothermia cases is whether critical brain hypoxia occurs before protective brain-cooling takes place
Effects of Hypothermia
Warming Methods
CPR and Drugs
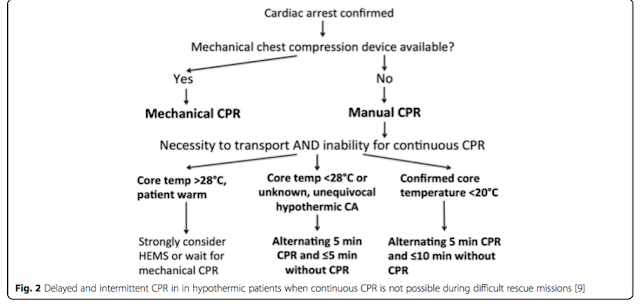
Mechanical chest compression devices (deliver >50 % of baseline cerebral blood flow in normothermia) are likely to provide sufficient oxygen delivery to vital organs in deeply hypothermic patients. When mechanical CPR is not available and manual CPR is not feasible, intermittent >CPR has been suggested.
International guidance differ on drug administration. ERC 2015 guidelines recommend withholding adrenaline administration in hypothermic CA (HT IV) and limiting defibrillation to three attempts until the core temperature is >30 °C. In contrast, American Heart Association guidelines allow further defibrillation attempts concurrent with rewarming strategies and state that it may be reasonable to consider adrenaline administration during CA according to the standard ALS algorithm.
Brain oxygen-consumption decreases by ~6 % per 1 °C fall in core temperature and reaches 16 % at 15 °C compared with normothermia. This improves the brain’s tolerance for low- or no blood-flow states.
Factors affecting the outcome of a hypothermic arrest
(1) hypoxia (the most important single factor)
(2) patient considerations (e.g. age, co-morbidities, trauma)
(3) speed of cooling
(4) environment (air, water, snow)
(5) CA features (body temperature; whether hypoxia preceded arrest; delay before instituting CPR, and CPR quality)
(6) rescue considerations (e.g. adequate training to manage a low flow or no blood-flow state; speed of hospital transfer)
(7) proximity of appropriate hospital facilities
(8) whether hospital staff appreciate the special requirements of these cases
At 18 °C the brain tolerates CA for up to 10 times longer than at 37 °C
Staging of Hypothermia
(1) hypoxia (the most important single factor)
(2) patient considerations (e.g. age, co-morbidities, trauma)
(3) speed of cooling
(4) environment (air, water, snow)
(5) CA features (body temperature; whether hypoxia preceded arrest; delay before instituting CPR, and CPR quality)
(6) rescue considerations (e.g. adequate training to manage a low flow or no blood-flow state; speed of hospital transfer)
(7) proximity of appropriate hospital facilities
(8) whether hospital staff appreciate the special requirements of these cases
Effects of Hypothermia
Warming Methods
CPR and Drugs
Mechanical chest compression devices (deliver >50 % of baseline cerebral blood flow in normothermia) are likely to provide sufficient oxygen delivery to vital organs in deeply hypothermic patients. When mechanical CPR is not available and manual CPR is not feasible, intermittent >CPR has been suggested.
International guidance differ on drug administration. ERC 2015 guidelines recommend withholding adrenaline administration in hypothermic CA (HT IV) and limiting defibrillation to three attempts until the core temperature is >30 °C. In contrast, American Heart Association guidelines allow further defibrillation attempts concurrent with rewarming strategies and state that it may be reasonable to consider adrenaline administration during CA according to the standard ALS algorithm.
The benefit of antiarrhythmic drugs in hypothermic CA is unclear. Many arrhythmias (e.g. bradycardia, atrioventricular blocks, atrial fibrillation, nodal rhythms and QRS prolongation with or without Osborn J-waves) are considered benign in accidental hypothermia, usually regress with patient rewarming and do not require further treatment provided the perfusion is deemed adequate. Most intravenous anaesthetic induction agents cause cardiovascular depression so doses should be small. Hypothermia reduces the systemic clearance of CYP450- metabolised drugs by an amount proportional to the fall in body temperature, increasing the likelihood of unanticipated toxicity.
Treatment Algorithm based on Staging and cardiopulmonary status
Further Reading
Paal P, Gordon L, Strapazzon G, Maeder MB, Putzer G, Walpoth B, Wanscher M, Brown D, Holzer M, Broessner G, Brugger H. Accidental hypothermia–an update. Scandinavian journal of trauma, resuscitation and emergency medicine. 2016 Dec;24(1):111.
Posted by:
Treatment Algorithm based on Staging and cardiopulmonary status
Further Reading
Paal P, Gordon L, Strapazzon G, Maeder MB, Putzer G, Walpoth B, Wanscher M, Brown D, Holzer M, Broessner G, Brugger H. Accidental hypothermia–an update. Scandinavian journal of trauma, resuscitation and emergency medicine. 2016 Dec;24(1):111.
Posted by:
Lakshay Chanana
ST4 Trainee
Royal Infirmary of Edinburgh
Department of Emergency Medicine
Edinburgh
Scotland





No comments:
Post a Comment